Apr 30, 2024 /
Behavioral Health
By Dusty Frisby-Housel / Summit
Navigating Postpartum Depression
The arrival of a new baby can bring on a whirlwind of emotions. From feeling joy and excitement to being overwhelmed, having some anxiety, and even experiencing some sadness—it’s a rollercoaster ride of emotions for parents. While it’s normal to experience a range of emotions after having a baby, it’s essential to recognize when something more serious, like postpartum depression (PPD), may be at play.
Postpartum depression is a serious mental health condition that can affect some mothers after childbirth. It typically occurs in the first six weeks following childbirth, but can develop anytime over the first year. Postpartum depression is more than just feeling down or worried; it can impact your ability to connect with and care for your baby and disrupt your daily life.
Postpartum depression rates are higher among mothers who have a history of anxiety or depression, a history of PPD, or are first-time mothers. In Utah, approximately one in eight new mothers are affected by postpartum depression.
While some parents may experience “baby blues,” which can involve feeling tearful, having a down or worried mood, and even crying spells, these symptoms come on shortly after birth and usually resolve within two weeks.
If these feelings persist for more than two weeks and interfere with your ability to function, it may be a sign of postpartum depression. Other signs of PPD may include:
Doctors often use tools like the Edinburgh Postnatal Depression Scale (EPDS) to screen for PPD. At Wasatch Pediatrics, your pediatrician will use this screening questionnaire when you bring your baby in at each well visit in the first six months of life. If concerns are identified, we’ll help provide resources or ask to share the results with your primary care provider or OB/GYN for further follow-up and treatment.
Fortunately, there are many resources and treatments available for postpartum depression. Whether it’s through your primary care provider, OB/GYN, or a mental health professional, there are many ways to support you through this challenging time. Options include counseling, support groups, new mom groups, and even medications that are safe while breastfeeding.
Additionally, making self-care a priority can also help alleviate symptoms. Simple activities like getting enough rest, asking your support system for help with caring for your baby or daily chores, talking to your partner, family, and friends about your feelings, talking to other new moms about your experience, and engaging in hobbies can all make a difference.
The SUNSHINE acronym below offers practical tips for self-care (*developed in partnership with the Utah Department of Health and Postpartum Support International Utah):
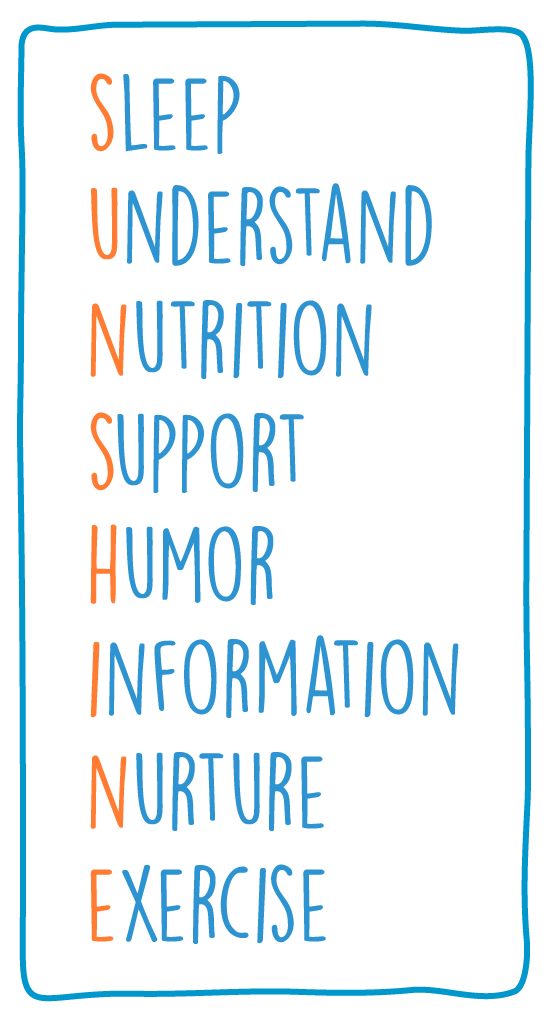
Sleep: Aim for four to six hours of sleep in a row, at least three nights a week.
Understand: Counseling with a trained maternal mental health professional prevents and treats mental health issues.
Nutrition: Take a prenatal vitamin through one year postpartum. Avoid caffeine and sugar when possible. Include protein and unsaturated fats at every snack and meal. Drink two large pitchers of water daily.
Support: Share your feelings with a trusted friend or family member or find a support group online or in-person. Ask for help with baby care – getting an hour each day to yourself is essential.
Humor: Make time for silliness and joy each day. A funny movie, time with friends, or tickling your children can all improve your mood. If laughing seems impossible, it is time to seek more support.
Information: Consult the Edinburgh Postnatal Depression Scale monthly for a year postpartum to track your mental health. Call your provider if your score is 10 or above, or if you marked anything other than “never” on question 10 about self-harm.
Nurture: Care for yourself through nature, spiritual practices, music and art, meditation, dates with friends, etc. Schedule weekly time in your calendar to do things you enjoy outside of motherhood.
Exercise: Walking 10 – 20 minutes a day can help your body, mind, and spirit heal and stay emotionally healthy. You can also try yoga or stretching if your provider gives you the go-ahead.
If you are experiencing (or think you may have) postpartum depression, please call your primary care provider, OB/GYN, or midwife.
Resources you can use without a referral include:
Remember, you’re not alone, and help is available. By recognizing the signs of postpartum depression and seeking support early on, you can take the first steps toward healing, recovery, and feeling better.
©2026 Wasatch Pediatrics